How does dual coverage work?
It's not uncommon to have coverage under two dental plans. For example, your children may have dental benefits through your employer and your spouse's employer. Anyone with dental coverage under two separate plans has dual coverage.
How it works
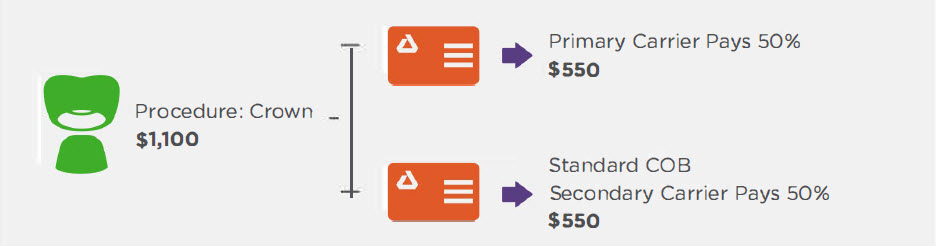
The way benefits carriers work together when a person has dual coverage is called coordination of benefits or COB. Dual coverage does not mean double benefits. For example, if both of your plans cover two cleanings per year, having dual coverage won't provide coverage for four cleanings. Here's how it works:
| 1 | 2 | 3 |
|---|---|---|
| The dentist bills the primary benefits carrier. The primary carrier pays its portion. | The remainder of the bill is sent to the secondary benefits carrier. In some cases, the secondary carrier may cover the rest of the bill, reducing your out-of-pocket costs. | The remainder (if any) is your responsibility. |
An exception to the rule: Some dental plans have a non-duplication of benefits clause. This rule prevents secondary plan coverage if the primary plan already paid as much or more than the secondary plan would have covered had it been primary. Check your plan information to see if your secondary plan has this rule before using your benefits.
Determining which plan is primary
| For yourself: | For yourself, if you have two jobs: | For your children: | For children of divorced parents: |
|---|---|---|---|
| Your primary carrier is typically the coverage you receive through your employer. Additional coverage through a spouse will be secondary. | If you have dental benefits through both employers, the primary plan is usually the one that has provided coverage the longest. | The parent whose birthday falls first in the calendar year will have the primary plan. For example, if your birthday is August 9, and your spouse's birthday is July 21, your spouse's plan would be the primary plan. Birth year is not a factor. | Primary benefits are typically through the parent with the most custody, but can vary. |
The primary plan is the one billed first. The plan billed after the primary carrier has paid its portion is called the secondary plan. Which plan is primary varies by situation.
When both plans are Delta Dental plans
If your primary or secondary plan is a HMO-type plan (such as DeltaCare® USA), please contact your carrier for specifics on how dual coverage is handled.
 Download PDF
Download PDF

